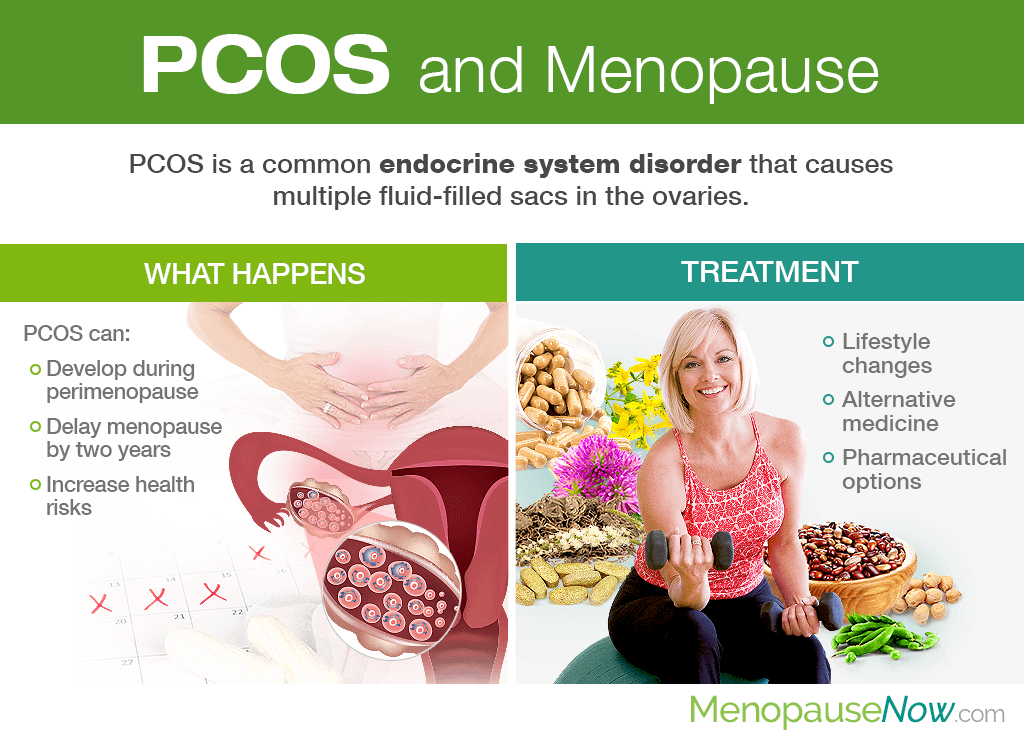
Polycystic ovary syndrome (PCOS) is a health condition that affects women of all ages. However, not much is known about the disorder as they woman reach and pass the end of her fertile years. Continue reading to learn more about PCOS and menopause, including its significance in the lives of peri- and postmenopausal women, how to treat PCOS during menopause, and more.
About PCOS
Polycystic ovary syndrome (PCOS) is a common endocrine disorder involving an imbalance of reproductive hormones that affects up to 10 percent of women of reproductive age.
The hormonal imbalance often causes multiple fluid-filled sacs (cysts) in the ovaries from eggs not developing or being released during ovulation as they normally do during a healthy menstrual cycle, hence the name polycystic ovary syndrome.
While the exact cause of PCOS is still under debate, most experts agree on a couple of principal factors playing an important role in the condition's development, including high androgen levels and elevated insulin levels.
Some of the most common PCOS symptoms - greatly universal across women's reproductive stages - are irregular periods; hirsutism; skin tags; female-patterned baldness that involves hair loss on the scalp; darkening of the skin; weight gain; acne; and more.
PCOS and Menopause
There is a wide range of information to know about PCOS and menopause, starting with responses to some of the most commonly asked questions.
Can PCOS Develop during Menopause?
Women commonly find out they have PCOS in their 20s and 30s when they are having fertility issues. However, PCOS can happen at any age after puberty. As such, it is not uncommon for PCOS to develop as a woman is passing through the menopause transition.
How Is It Possible to Develop PCOS during Menopause If Hormone Levels Decrease?
Even with the reduction in estrogen and progesterone levels when the ovaries wind down reproductive function, women may still have excess testosterone levels that drive the hormonal imbalance behind the endocrine disorder.
I Have PCOS Since Premenopause. Does It Continue Into Menopause?
It is possible for women to enter menopause with PCOS.
Interestingly enough, many perimenopausal women with PCOS find that their irregular periods begin to normalize as they get closer to their menopause date. Also, it is not uncommon for women with PCOS to reach menopause two years later than their non-PCOS counterparts.
What are My Health Risks as a Menopausal Woman with PCOS?
There are certain health risks that all women with PCOS are susceptible to, including, but not limited to:
- Diabetes
- Chronic inflammation
- Cardiovascular problems, such as stroke, high blood pressure, and unhealthy cholesterol levels
- Sleep apnea
- Depression and anxiety
- Obesity
- Endometrial cancer
While yes, many midlife women are at risk for some of the aforementioned conditions, like weight gain, depression, stroke, and anxiety, menopausal women with PCOS need to be extra wary.
Can PCOS Continue After Menopause?
Studies suggest that elevated testosterone levels do not decrease until 20 years into postmenopause if not properly addressed, meaning that symptoms and health risks can still haunt your days long after your last period.
Treatment of PCOS during Menopause

Some of the first measures toward preventing or treating PCOS during menopause include making lifestyle adjustments that encourage hormonal balance before considering pharmaceutical options, such as low-dose birth control or anti-androgen drugs like spironolactone.
Menopause symptoms treatments promote a well-balanced diet with foods rich in phytoestrogens as well as the essential macronutrients - lean protein, healthy fats, and complex carbs. Women with PCOS should avoid overconsumption of simple sugars by all means as this may exacerbate already high insulin levels.
Women with PCOS should also aim to participate in regular exercise of at least 30 minutes a day, five days a week as it can help with weight control. If not able to perform all of the required time in one setting, break it up into sessions throughout the day as needed.
Moreover, it is crucial to partake in wholesome habits for hormonal health, which includes quitting smoking, tobacco, excessive caffeine consumption, etc. To relieve pent-up tension, try stress-reduction techniques of yoga, meditation, tai chi, or a favorite hobby.
To directly tackle the root cause, hormonal imbalance, consider pairing these approaches with alternative medicine used to bring reprieve from PCOS and other menopause symptoms. They include phytoestrogenic herbal supplements and hormone-regulating supplements.
Phytoestrogenic herbal supplements
Phytoestrogenic herbal supplements contain higher concentrations of phytoestrogens that fill an estrogen deficit in the body. They famously include black cohosh, red clover, dong quai, and St. John's wort, among others.
Although beneficial in relieving menopause symptoms, they may not be the best option for PCOS as they do not directly address the testosterone excess. Also, introducing exogenous hormones into the body may promote dependence. Use them with caution and under the supervision of a certified herbalist.
Hormone-regulating supplements
On the other hand, hormone-regulating supplements, like Macafem, stimulate and encourage the endocrine system glands to produce more of their own hormones, thus balancing levels.
By doing so, women may resolve PCOS during menopause without the need for introducing outside hormones into the body. Likewise, women can finally find relief from their menopause symptoms, essentially treating two problems with one solution.
Sources
- Healthy Women. (n.d.). PCOS and Menopause. Retrieved May 28, 2019, from https://www.healthywomen.org/content/article/pcos-and-menopause
- Lenart-Lipinska, M. et al. (2014). Polycystic ovary syndrome: clinical implication in perimenopause. Przegla̜d Menopauzalny, 13(6), 348-351. doi: 10.5114/pm.2014.47988
- Minooee, S. et al. (2018). Prediction of age at menopause in women with polycystic ovary syndrome. Climacteric, 21(1), 29-34. doi: 10.1080/13697137.2017
- Office on Women's Health. (2019). Polycystic ovary syndrome. Retrieved May 28, 2019, from https://www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome