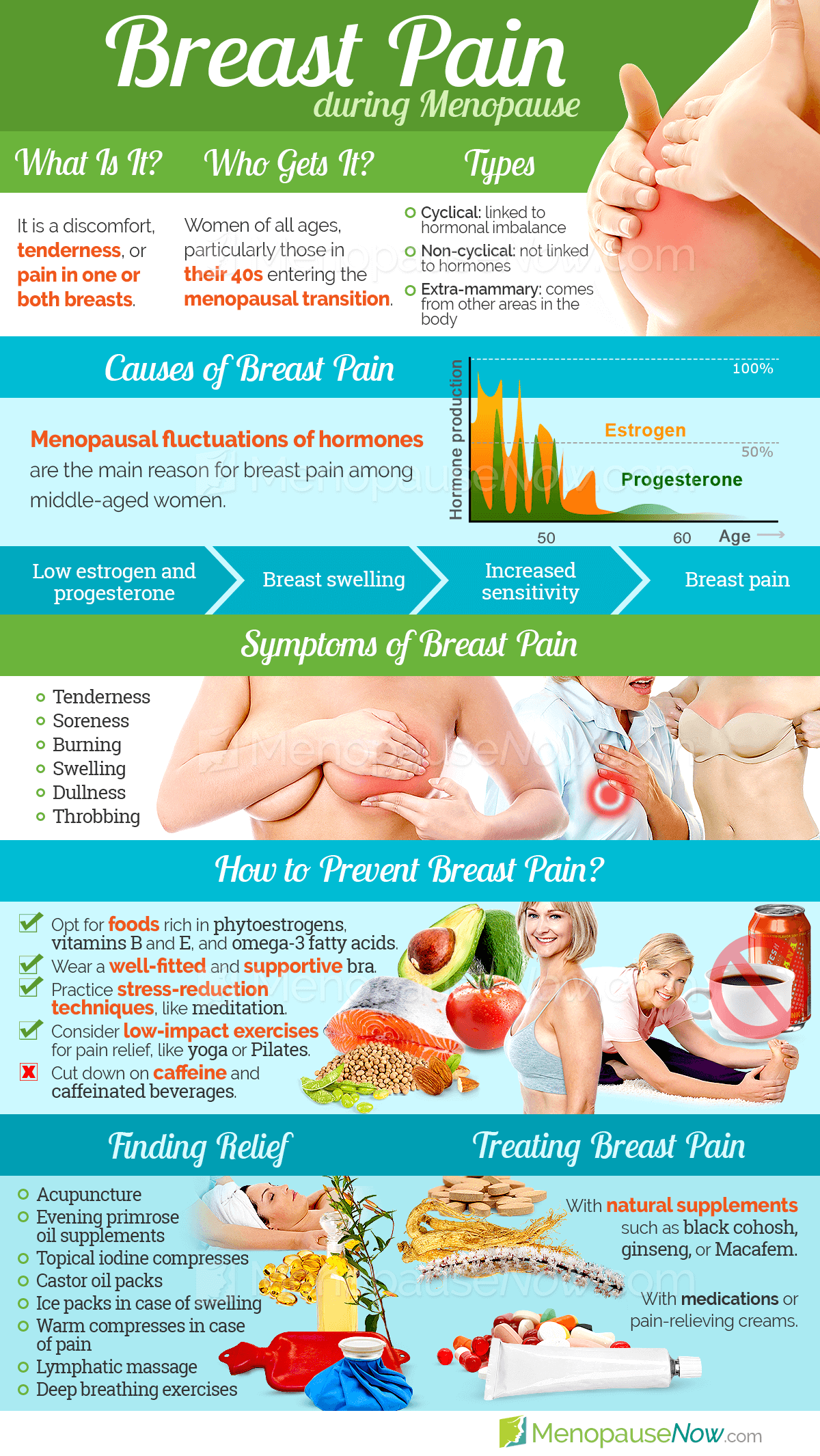
Breast pain is a common symptom that can develop during the menopausal transition due to fluctuating estrogen and progesterone levels. While postmenopausal women can experience breast pain, it is most common in premenopausal and perimenopausal women.
A common complaint, breast pain affects as many as 70% of women at some point in their lives. Only a small portion of these women, about 10%, will experience severe breast pain, which can negatively impact relationships, work, and daily life. Nevertheless, breast pain can prompt understandable questions and concerns at any intensity.
Understanding menopausal breast pain is one of the best steps toward managing this symptom. Read on to learn more about breast pain.
About Breast Pain
Breast pain - known medically as mastalgia, mastodynia, and mammalgia - is the general term used to mean discomfort, tenderness, or pain in one or both of the breasts.
Breast pain is categorized as either cyclical or non-cyclical. With the former, breast pain is the result of hormonal changes, making it the most common kind of breast pain in pre- and perimenopausal women. Non-cyclical breast pain, more common in postmenopausal women, is not related to hormonal changes. Extramammary breast pain, which originates outside the breast, is a third type of breast discomfort.
Breast pain symptoms can vary depending on the type and the individual woman. Generally speaking, symptoms include tenderness, tightness, soreness, burning, swelling, dullness, and aching. Symptoms can be consistent or intermittent and may affect one or both breasts.
Click here to learn more about breast pain, or read on to learn more about the causes of breast pain.
Causes of Breast Pain
The most common cause of breast discomfort during menopause is hormonal change. As with all times of hormonal fluctuation, like menstruation and pregnancy, menopause can alter the levels of estrogen and progesterone in the body. As a result, women may develop breast pain.
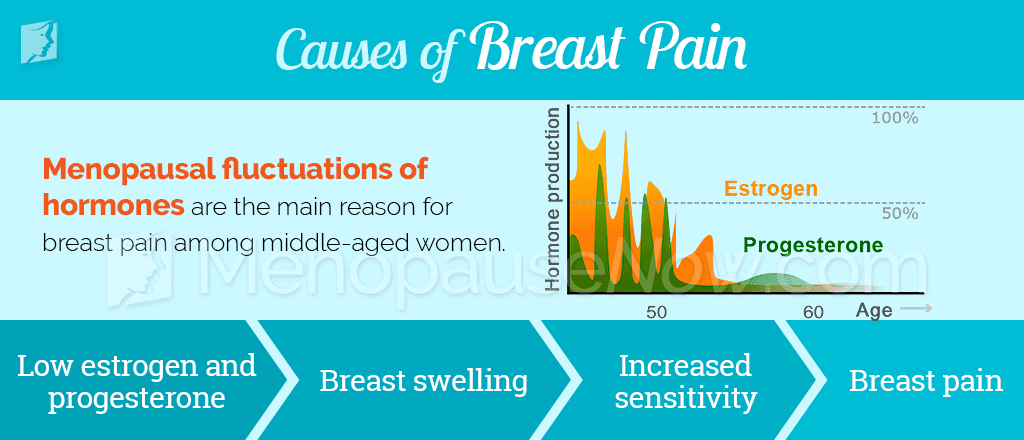
While hormones are the most common cause of breast pain experienced in menopause, other factors can cause or contribute to breast pain. These rarer causes range from serious health conditions to dietary issues.
- Breast cysts
- Breast trauma
- Prior breast surgery
- Breast size
- Stress
- Alcoholism
- Oral contraceptive use
- Antidepressants
- Mastitis
- Hormone replacement therapy (HRT)
- Cholesterol and heart drugs
Click here to learn more about the causes of breast pain, or read on to learn more about when to speak with a doctor about breast pain.
Breast Pain Diagnosis

While breast discomfort during menopause is not usually cause for alarm, it is never a bad idea to consult a doctor about this symptom. Though breast pain is rarely indicative of cancer, speaking with a doctor to rule out breast cancer can greatly help allay these worries and help a woman determine the best way to manage breast tenderness.
Women who experience prolonged and unexplained breast pain or additional accompanying symptoms should speak with a doctor to rule out rare, but more serious, causes of breast pain. At a doctor visit, a full physical and clinical exam will be performed. If something more serious is suspected, a doctor may order additional tests.
Click here to learn more about breast pain diagnosis, or continue reading to learn more about the different breast pain treatments available.
Breast Pain Treatments
Fortunately, a number of self-care measures and natural treatments can help to relieve breast pain during menopause with little or no risk of side effects. Self-care can include regular exercise, massage, relaxation techniques, and avoidance of dietary and lifestyle triggers.
While these can help a woman reduce the severity of breast pain, they alone cannot solve the root problem of hormonal imbalance. Alternative therapies are safe and effective methods of relieving breast pain symptoms by targeting the root cause of hormonal imbalance. A majority of women find that a combination of self-care and natural therapies is the best way to address breast pain in menopause.
Experts recommend exploring medical options only after these other methods have failed to provide relief, because these are often more invasive and carry greater risks.
Click on the following link to learn specific treatments for breast pain, which begin with lifestyle changes, move onto alternative medicines, and finally, if those options don't seem to help, prescription medications. The most effective treatments for breast pain typically combine lifestyle changes and alternative medicines.
Sources
- Love, S. (2003). Menopause and Hormone Book. New York: Three Rivers Press.
- National Health Service UK. (2014). Breast pain. Retrieved April 15, 2016, from http://www.nhs.uk/conditions/breastpaincyclical/Pages/Introduction.aspx
- Office on Women's Health. (2012). Menopause and menopause treatments fact sheet. Retrieved April 15, 2016, from http://www.womenshealth.gov/publications/our-publications/fact-sheet/menopause-treatment.html