Women who ask how is menopause diagnosed are colloquially referring to perimenopause, which is a transformative, years-long transition leading up to menopause, or the date that marks 12 consecutive months without a period. As perimenopause is considered a milestone in the lives of many, women may wonder how exactly they can confirm its arrival.
Continue reading to learn all about the menopause diagnosis, including various diagnostic tests for menopause, as well as what to do next for symptom treatment.
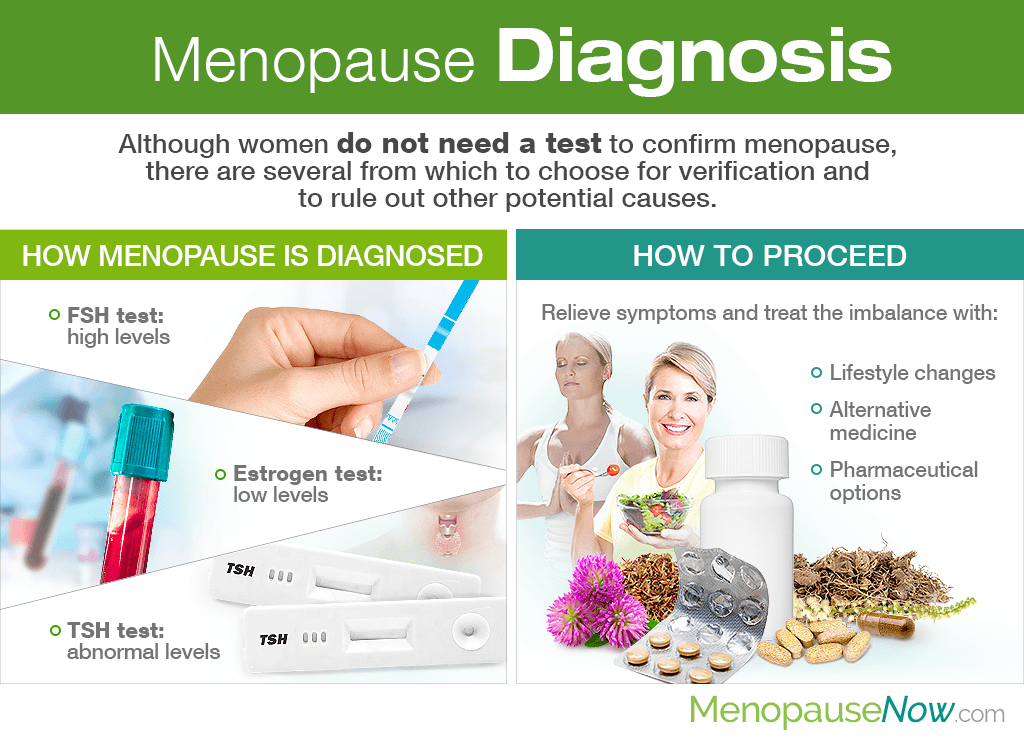
How Menopause is Diagnosed
Generally, a woman does not need to perform a test to confirm that she has entered the menopausal transition, and no one test or sign is enough to determine the official beginning either.
When diagnosing perimenopause, doctors take into consideration menstrual history, age, and any menopause symptoms or body changes she may be experiencing.
Nevertheless, there are several diagnostic tests for menopause that doctors can order to verify that she has, indeed, entered perimenopause. They include:
Follicle stimulating hormone (FSH) Test

Levels of follicle stimulating hormone (FSH), which is produced by the pituitary gland, increase temporarily each month to stimulate ovaries to mature eggs. As a woman enters perimenopause, the hormone's levels tend to increase in attempt to make the ovaries produce more estrogen.
Estrogen Test
Drastic fluctuations are characteristic of perimenopause as the ovaries wind down reproductive functions. As such, an estrogen test that serves as diagnosis of perimenopause may prove to find lower than normal levels of the hormone.
Thyroid stimulating hormone (TSH) Test
Whereas, a menopause differential diagnosis may include a TSH test in order to rule out a thyroid problem, whose symptoms are similar to those of perimenopause and may include irregular periods, hot flashes, mood swings, and fatigue, among others.
How to Proceed

What comes next after a positive perimenopause diagnosis will depend on the woman, as each woman experiences the menopause transition differently.
In general, women are encouraged to pursue less risky menopause symptoms treatments first, which encourage overall endocrine system health. They include the implementation of lifestyle changes alongside alternative medicine. Pharmaceutical options may also be considered as a last resort.
Lifestyle changes
Lifestyle changes involve the least risk, yet most discipline. Nevertheless, when partaken in continually, their benefits are abundant. Try the following:
Optimize your diet. A low-fat, high-fiber diet to promote gastrointestinal health and ward off cardiovascular problems should be of high priority. Also, consume foods rich in calcium and vitamin D for optimal bone health as well as phytoestrogens, plant-based estrogens that act as the natural hormone in the body. Fresh fruits and vegetables; whole grains; legumes; and omega-3s-rich fatty fish are all viable options.
Stay active. Regular exercise has been shown to elevate mood, prevent weight gain, encourage healthy sleeping patterns, strengthen bones, and more. Try to partake in aerobic and weight-bearing exercises - walking, dancing, jogging, etc. - for 30 minutes a day, five days a week. If necessary, work with a personal trainer for optimal results.
Practice wholesome habits. Excess stress can throw hormonal balance further out of line, thus leading to thyroid and adrenal dysfunction. Take time to unwind each day with yoga, meditation, tai chi, aromatherapy, deep breathing exercises, and other stress-relief techniques. Also, quit addictions to tobacco, caffeine, alcohol, and others that could further aggravate endocrine health.
Alternative medicine
Two alternative medicine options have been renowned for their effectiveness in promoting hormonal balance throughout and after the menopause transition. They are:
Phytoestrogenic herbal supplements. Phytoestrogenic herbal supplements, like black cohosh and red clover, contain potent concentrations of phytoestrogens, more so than their dietary counterparts. As such, they directly combat an estrogen imbalance. Use them short-term as extended use can lead to dependence.
Hormone-regulating supplements. Hormone-regulating supplements, such as Macafem, encourage the pituitary glands to produce more of their own natural hormones, thus resolving a hormonal imbalance causing menopause symptoms without the unnecessary introduction of exogenous hormones into the body. Because of this, they can be used long-term.
Pharmaceutical options
Speak with your doctor about pharmaceutical options, like hormone replacement therapy (HRT), if aforementioned measures don't work. Keep in mind that their use can include serious risks and side effects that may be worse than the symptoms one is trying to treat.
Key Takeaways
In sum, no one diagnostic test for menopause is sufficient to confirm that a woman has entered perimenopause. Various factors - including menstrual history, age, and symptoms - are taken into consideration. Nonetheless, FSH, TSH, and estrogen tests may also lead to a glimpse of what's going on insider of her body.
Luckily, there are several measures women can pursue to allay symptoms and ultimately treat the hormonal imbalance taking place. They start, principally, with lifestyle changes and alternative medicine. If these less risky options don't provide relief, pharmaceutical options may be pursued with caution and under the supervision of a trusted healthcare professional.
Sources
- Harvard Health Publishing. (2009). Perimenopause: Rocky road to menopause. Retrieved August 20, 2019, from https://www.health.harvard.edu/womens-health/perimenopause-rocky-road-to-menopause
- Martin, K.A. & Manson, J.E. (2008). Approach to the Patient with Menopausal Symptoms. The Journal of Clinical Endocrinology & Metabolism, 93(12), 4567-4575. doi: 10.1210/jc.2008-1272
- Mayo Clinic. (2017). Menopause: Diagnosis & treatment | Perimenopause: Diagnosis & treatment. Retrieved August 20, 2019, from https://www.mayoclinic.org/diseases-conditions/menopause/diagnosis-treatment/drc-20353401 | https://www.mayoclinic.org/diseases-conditions/perimenopause/diagnosis-treatment/drc-20354671
- National Collaborating Centre for Women's and Children's Health (UK). (2015). Diagnosis of perimenopause and menopause. Retrieved August 20, 2019, from https://www.ncbi.nlm.nih.gov/books/NBK343466/
- The North American Menopause Society. (n.d.). How Do I Know I'm in Menopause? Retrieved August 20, 2019, from https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/how-do-i-know-i%27m-in-menopause-
- Ranabir, S. & Reetu, K. (2011). Stress and hormones. Indian Journal of Endocrinology and Metabolism, 15(1), 18-22. doi: 10.4103/2230-8210.77573