Perimenopause is the period that leads up to menopause, beginning when a woman first starts noticing symptoms and ending when she has not had a period for an entire year. There are many reported symptoms of perimenopause, one of which is a feeling of depression. If not treated when it first arises, depression can develop into a clinical condition. Read on to learn ways to deal with depression during perimenopause.
What Is Depression?
Depression is a chronic state of sadness, sometimes triggered by seemingly trivial things, difficult circumstances, or for no obvious reason. It is more than just feeling sad as a natural human response to a distressing event. It generally does not easily fade on its own, and someone who experiences depression may not be able to just "snap out of it." It can cause physical symptoms as well, such as exhaustion from simple daily activities.
Why Does Menopausal Depression Occur?
There are a few possible reasons for perimenopausal depression that can often accumulate.
Hormonal fluctuations
Estrogen interacts with the part of the brain that controls mood, regulating the activity of the natural mood elevators endorphins and serotonin. As perimenopause is a time of fluctuating estrogen production that is gradually declining, it is no surprise that temperament can be disrupted.
Other menopause symptoms
Other symptoms of menopause (e.g., hot flashes, sleep problems, and vaginal dryness) can be painful, embarrassing, and distressing, and they can have an understandable effect on overall well-being and mood.
Stressful life events
The timing of perimenopause tends to coincide with other big changes in a woman's life, such as aging parents, death of a spouse, or children leaving home. For obvious reasons, these can add up and contribute to depression.
Dealing with Depression
The good news is that depression does not have to be an inevitable part of perimenopause. The first place to start is to develop good lifestyle habits. A few possibilities are outlined below.
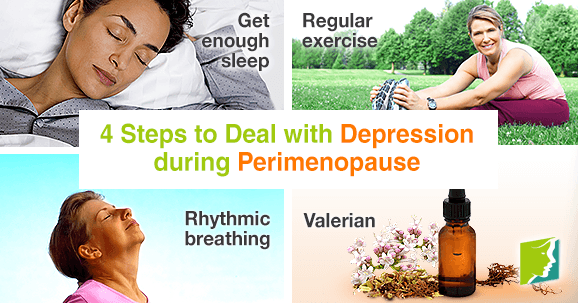
Get enough sleep
Lack of sleep can cause you to think irrationally, and getting into a cycle of negative thoughts will only worsen depression. Sleeping in a cool, dark, quiet room and going to bed at roughly the same time every night both encourage better sleep. If this is not possible, however, or you have tried this and are still not sleeping, talk to a doctor. He or she should be able to help you with insomnia.
Regular exercise
Serotonin and endorphins are released into the body during exercise, so physical activity can provide long-term prevention against depression. It can also reduce negative feelings in a person already suffering from depression.
Rhythmic breathing
Rhythmic breathing can help reduce anxiety and upset feelings. Slowly breathe in and then exhale, paying attention to your body's natural relaxation response. The key is to breathe deeply and from the abdomen. This simple act of focusing on relaxation can improve depression and negative thought patterns. Spending around 10 - 15 minutes a day doing these exercises should clear your mind and help bring down your stress levels.
Valerian
Containing the natural relaxants valerenic acid and valeranon, valerian can help combat stress and low mood. It also helps promote better sleeping patterns, which will lead to less fatigue and irritability. However, care must be taken not to take this herb for more than a few weeks at a time or at the same time as other sleep-inducing medications.
Depression during perimenopause can negatively affect all areas of life, including work and relationships. For this reason, it is important to take steps to reduce it as early as possible. If depression persists, talking to a doctor will help you decide the right treatment for you, whether that be advice from local services, medical treatment, or other therapies.
For more information on depression and how to treat it, follow the links below.
Sources
- Anxiety UK. (n.d.). Guide to herbal medicines. Retrieved March 1, 2016, from https://www.anxietyuk.org.uk/get-help/get-help-3/guide-to-herbal-medicine
- Kahn, D.A. et al. (n.d.). Depression during the transition to menopause: A Guide for Patients and Families. Retrieved March 1, 2016, from http://womensmentalhealth.org/wp-content/uploads/2008/04/menopause_guide.pdf
- National Health Service UK.(2012). Clinical depression. Retrieved August 25, 2014, from http://www.nhs.uk/Conditions/Depression/Pages/Introduction.aspx
- National Health Service UK. (2014). Clinical depression - Symptoms. Retrieved March 1, 2016, from http://www.nhs.uk/Conditions/Depression/Pages/Symptoms.aspx
- Shors, T.J. & Leuner, B. (2003). Estrogen-mediated effects on depression and memory formation in females. Journal of affective disorders, 74(1), 85-96. Retrieved August 25, 2014, from http://www.ncbi.nlm.nih.gov/pubmed/12646301
- University of Maryland Medical Center. (2015). Depression. Retrieved March 1, 2016, from http://umm.edu/health/medical/altmed/condition/depression