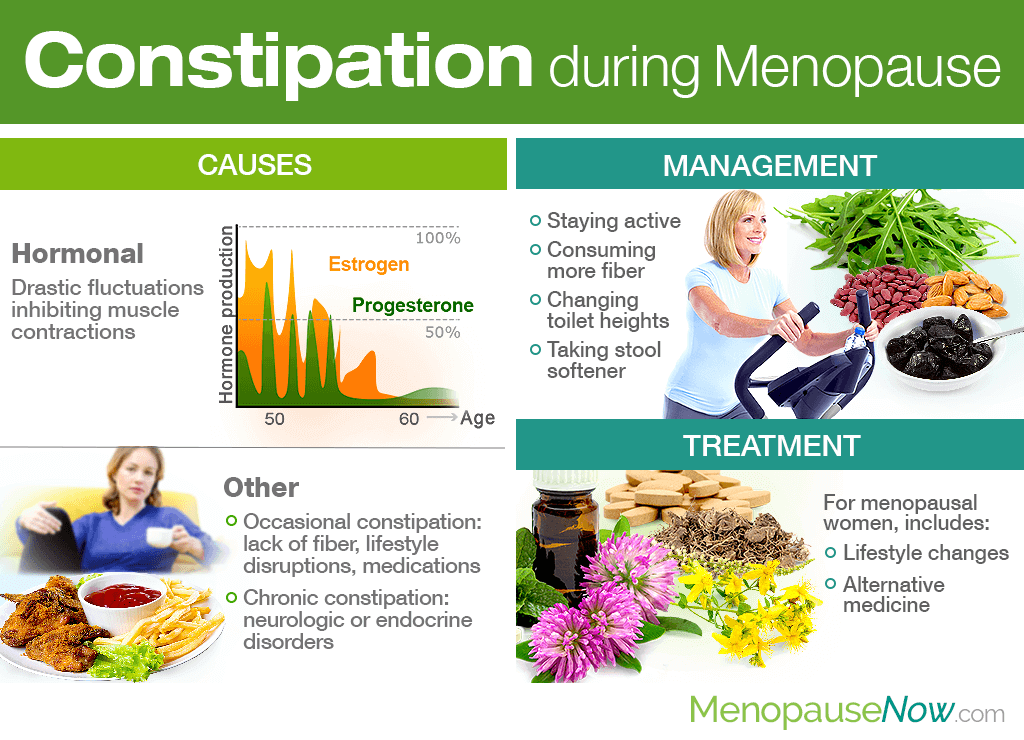
As if hot flashes, night sweats, and mood swings weren't enough, it is not uncommon for women to suffer from constipation during perimenopause as well. Luckily, this symptom does not have to plague their days for years to come.
Continue reading to learn all about constipation during menopause, including its causes, management techniques, and treatment options for ultimate relief.
Why Does It Happen?
Constipation during perimenopause can happen for a variety of reasons; however, the most common is due to hormones.
Hormonal causes
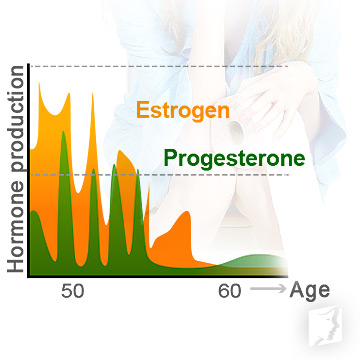
While research is still developing, it is believed that drastic hormonal fluctuations are the reason behind constipation and other digestive problems in women passing through perimenopause.
Estrogen and other ovarian hormone receptors have been found in the gastric and small intestinal mucosa, and these female sex steroid hormones inhibit muscle contractions in the colon when they are imbalanced, thus causing instances of constipation.
Other causes

Other causes of occasional constipation during perimenopause include inadequate dietary fiber, lifestyle disruptions such as hospitalizations, changes in sleeping habits, or travel; lack of exercise; or medications.
Likewise, causes of chronic constipation include neurologic disorders - such as Parkinson's disease, strokes, multiple sclerosis (MS), or spinal cord injuries - or endocrine disorders, like diabetes and hypothyroidism.
How Can I Manage Constipation during Menopause?

There are several measures women can pursue in order to manage constipation during perimenopause, including:
- Staying active. Strive for cardio, yoga, or pelvic floor exercises to ease constipation during menopause. They encourage peristalsis, the movement of food through the guts, and also encourage endocrine system health for optimal well-being.
- Revising your medicine cabinet. Sometimes, constipation leading into menopause is not due to hormonal influences, but to medicines a woman may be taking. If that is so, work with your doctor to address the issue and find possible replacements.
- Consuming more fiber. Insoluble fiber can help your constipation during menopause since it adds bulk to feces and quickens the passage through the guts. Foods such as prunes, nuts, seeds, beans, peas, and raw vegetables all contain insoluble fiber.
- Performing physical stimulation. Abdominal massages and perineal self-acupressure, which is when one presses the area that lies between the anus and vaginal opening, are two common techniques used by those suffering from fewer bowel movements.
- Changing toilet heights. When you squat over the toilet with your knees raised above your hips, this reflexively relaxes the pelvic floor. Toilets that do not allow this position - known as “comfort-height toilets” - make it harder to have a bowel movement. Consider putting a small stool under the feet when sitting on a comfort-height toilet.
- Taking stool softener. Stool softener is used as a final resort once other lifestyle changes have not worked. Over-the-counter stool softeners and laxatives like polyethylene glycol, docusate, or senna are popular options. Use as directed.
How Do I Treat the Symptom?

While aforementioned management techniques will help women stave off the menopause symptom short-term, long-term relief is found by treating the underlying cause, which is often hormonal imbalance.
Treatments for digestive problems such as constipation focus first on instilling lifestyle changes that alleviate intestinal issues while also leading to overall better health. Aside from regular exercise and increased fiber intake, menopausal women are also encouraged to consume foods rich in phytoestrogens, plant-based estrogens that boost hormones levels.
Furthermore, women are recommended to pair these lifestyle adjustments with alternative medicines that are proven to foster hormonal balance. They include phytoestrogenic herbal supplements and hormone-regulating supplements.
Phytoestrogenic herbal supplements contain stronger phytoestrogens than food alone and include preparations made from black cohosh, red clover, St. John's wort, and others. However, since they introduce exogenous hormones into the body, they are not recommended for long-term use.
On the other hand, hormone-regulating supplements, such as Macafem, nourish the thyroid and pituitary glands to produce their own hormones, thus alleviating constipation and other hormonal imbalance symptoms, like hot flashes, mood swings, vaginal dryness, and more. Because they do not contain hormones, they are safer for long-term use.
For constipation during menopause that is not caused by hormones, speak with your healthcare provider to properly diagnose the underlying condition and find alternative options.
Sources
- Academy of Nutrition and Dietetics. (2013). Constipation, Diarrhea and Fiber. Retrieved April 30, 2019, from https://www.oncologynutrition.org/erfc/eating-well-when-unwell/chemotherapy/constipation-diarrhea-and-fiber
- Cleveland Clinic. (2017). What Will Help You With Constipation After Menopause? Retrieved April 30, 2019, from https://health.clevelandclinic.org/what-really-works-for-your-constipation-after-menopause/
- Harvard Health Publishing. (2016). Coming to terms with constipation. Retrieved April 30, 2019, from https://www.health.harvard.edu/digestive-health/coming-to-terms-with-constipation
- Oh, J. et al. (2013). Estrogen Rather Than Progesterone Cause Constipation in Both Female and Male Mice. The Korean Journal of Physiology & Pharmacology, 17(5), 423-426. doi: 10.4196/kjpp.2013.17.5.423