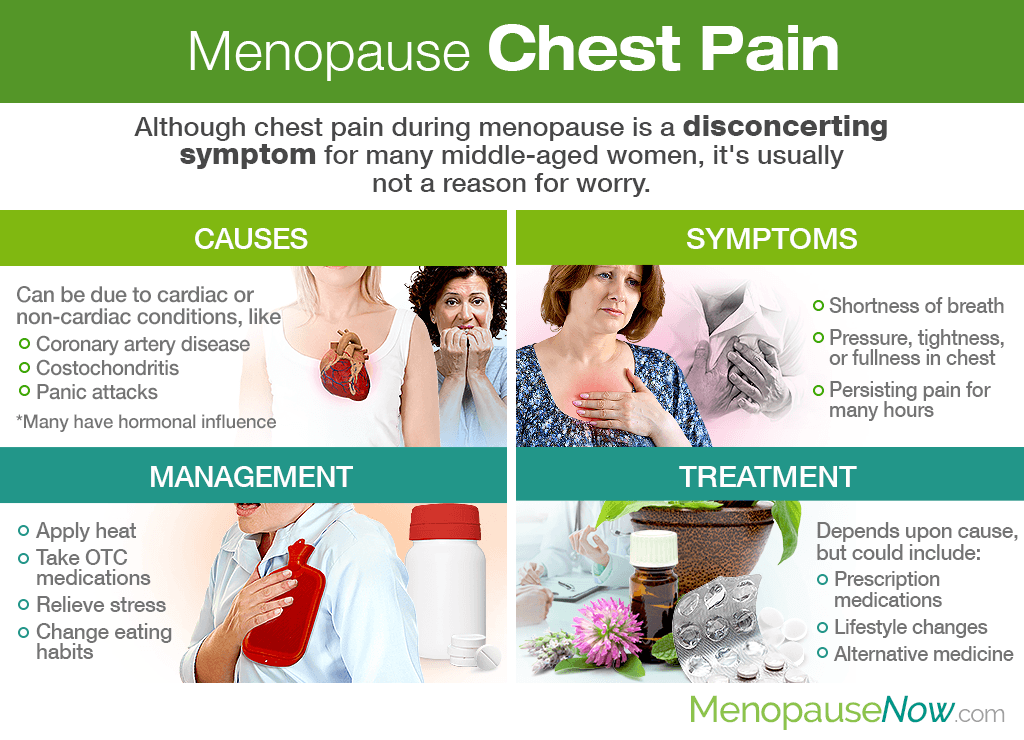
Chest pain during menopause is a disconcerting symptom for many middle-aged women, leaving them trying to figure out its origin and exactly what they can do before circumstances worsen. Luckily, discovering the underlying cause and appropriate solution for long-lasting relief is not far from reach. Continue reading to learn more about menopause and chest pain, including its many causes, symptoms, management techniques, and treatment options.
Causes of Menopause Chest Pain

Menopause chest pain can have cardiac or non-cardiac roots.
Cardiac Causes
Menopause is a transformative time during which a woman's ovaries are winding down reproductive functions as she enters her infertile years, provoking drastic variations in key hormones like estrogen and progesterone.
These hormonal changes can lead to cardiac conditions that cause chest pain as a symptom. They include, but are not limited to:
Arrhythmia. Fluctuating estrogen levels can provoke arrhythmias, also known as irregular heartbeat. Besides the heart beating too fast, too slowly, or skipping a beat, symptoms of arrhythmia can also include dizziness, shortness of breath, and chest pain or tightness.
Coronary artery disease (CAD). Natural menopause can be seen as a risk factor for CAD as fluctuating estrogen levels contribute to the unhealthy balance of cholesterol levels.1 When the arteries become hardened and narrowed due to the buildup of plaque (atherosclerosis), CAD can occur.
Heart attack. A middle-aged woman's biggest fear may be that she is having a heart attack, especially since the occurrence's most common symptom is chest pain in women.2 If accompanied by lightheadedness, shortness of breath, or a discomfort that radiates to the arms, back, stomach, neck, or jaw, seek medical attention immediately.
Non-Cardiac Causes
There are also other non-cardiac conditions that could provoke chest pain in middle-aged women passing through menopause, including issues that affect the digestive system, muscles, lungs, and more.
Within these conditions, fluctuating hormones may also play a role. Some of them are:
Heartburn. This uncomfortable burning sensation in the chest is a symptom of stomach acid washing up to the esophagus, also known as acid reflux during menopause.
Gallbladder or pancreas problems. Abdominal pain from such health conditions can radiate to the chest area, causing discomfort.
Costochondritis. Costochondritis is an inflammation of cartilage in the chest without the presence of swelling. Its cause is largely unknown, yet it is not due to heart or lung issues.
Sore muscles. Fibromyalgia and other chronic pain syndromes can produce persistent feelings of chest pain.
Panic attacks. Suffering from a panic attack - or panic disorder - is often accompanied by palpitations, sweating, shortness of breath, nausea, dizziness, and chest pain, among others.
Depression. Studies have found that those with depression are three times more likely to experience frequent chest pain than those who were not depressed, proving that depression can manifest itself as physical changes in the body.3
Symptoms of Menopause Chest Pain

Symptoms associated with cardiac chest pain during menopause include:
- Shortness of breath
- Cold sweats
- Dizziness
- Weakness or fatigue
- Nausea or vomiting
- Pressure, tightness, or fullness in the chest
- Pain that worsens with activity or comes and goes, varying in intensity
Depending on its cause, a few commonly reported symptoms associated with non-cardiac chest pain are:
- A sour taste or sensation of food re-entering the mouth (heartburn)
- Trouble swallowing
- A pain that increases with deep breathing or coughing
- Pain that persists for hours upon end
- Pain that improves or worsens when changing body positions
- A feeling of tenderness when the chest is pushed or touched
It is important that women who experience any kind of chest pain seek help immediately for appropriate diagnostic testing in order to rule out life-threatening causes.
Management Techniques

Effectively managing non-cardiac chest pain during menopause will also depend upon what is causing the irregularity to begin with.
Nevertheless, practical approaches could include:
Apply heat. Consider applying a wet, hot compress or heating pad to the area to ease any chest discomfort.
Do not overwork yourself. Women suffering from any type of menopause chest pain should avoid any aggravating activities, such as lifting heavy weights, exercising intensely, etc.
Take OTC medications. Over-the-counter pain relievers - like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) - may help relieve any temporary discomfort. Use any drugs with caution.
Relieve stress. Some non-cardiac chest pain is associated with excess stress levels, which can also negatively affect endocrine system health. Take time each day to meditate, practice yoga, or partake in a favorite hobby. Speaking with a therapist may also help.
Change eating habits. For those whose perimenopause chest pain is due to heartburn, eat smaller meals more often. Also, take your time while eating, and avoid triggers, such as garlic, black pepper, and citrus fruits.
While aforementioned measures may bring temporary relief, a long-term solution may only be found once the underlying cause is treated.
Treatment Options

Similar to other menopause symptoms, treating chest pain will widely depend upon what is causing the discomfort.
For cardiac-related chest pain, appropriate medications might be necessary to address the root cause of the problem, which could include aspirin or artery relaxers.
Also, because hormonal fluctuations are partly to blame for many of the menopause chest pain causes, middle-aged women would do well to pursue natural and effective menopause symptoms treatments that focus on promoting overall endocrine system health with lifestyle changes and alternative medicine.
Nevertheless, no matter the cause, it is crucial that women speak with their trusted healthcare providers in order to create a treatment plan that best fits their needs.
Key Takeaways
While there are many cardiac and non-cardiac conditions that can provoke menopause chest pain, one factor does stand tall as a common underlying culprit: drastic hormonal fluctuations. No matter the cause, is important that woman who feel any concerning symptoms report them immediately to a doctor for appropriate testing. While managing the pain can be as simple applying heat, relaxing, and trying not to over-exert yourself, long-term relief will only be found once the underlying cause is treated. In due time, your chest pain can disappear once and for all.
Sources
- British Heart Foundation. (n.d.). Menopause and your heart. Retrieved September 3, 2019, from https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/women/menopause-and-your-heart
- Cleveland Clinic. (2015). Non-Cardiac Chest Pain | Non-Cardiac Chest Pain: Management and Treatment. Retrieved September 4, 2019, from https://my.clevelandclinic.org/health/diseases/15851-gerd-non-cardiac-chest-pain | https://my.clevelandclinic.org/health/diseases/15851-gerd-non-cardiac-chest-pain/management-and-treatment
- Mayo Clinic. (2018). Chest pain: Symptoms & causes | Chest pain: Diagnosis & treatment. Retrieved September 3, 2019, from https://www.mayoclinic.org/diseases-conditions/chest-pain/symptoms-causes/syc-20370838 | https://www.mayoclinic.org/diseases-conditions/chest-pain/diagnosis-treatment/drc-20370842
- MedlinePlus. (2016). Arrhythmia | Coronary Artery Disease. Retrieved September 3, 2019, from https://medlineplus.gov/arrhythmia.html | https://medlineplus.gov/coronaryarterydisease.html
- National Institute on Aging. (2017). What Are the Signs and Symptoms of Menopause? Retrieved September 3, 2019, from https://www.nia.nih.gov/health/what-are-signs-and-symptoms-menopause
Footnotes:
- Cleveland Clinic. (2019). Estrogen & Hormones. Retrieved September 5, 2019, from https://my.clevelandclinic.org/health/articles/16979-estrogen--hormones
- American Heart Association. (2015). Heart Attack Symptoms in Women. Retrieved September 5, 2019, from https://www.heart.org/en/health-topics/heart-attack/warning-signs-of-a-heart-attack/heart-attack-symptoms-in-women
- Futurity. (2015). Depressed People Suffer Chest Pain More Often. Retrieved September 3, 2019, from https://www.futurity.org/chest-pain-depression-993722-2/