Perimenopause is the transitional period before a woman's last period, which signals the entrance into menopause and the end of fertility. This transitional phase is, for many women, the time when menopausal symptoms are at their worst. Hot flashes, mood swings, and stomach problems have all been reported.
Many women deal with irritable bowel syndrome (IBS) their whole lives, but oftentimes, this condition is found to worsen during the menopause transition. To find out how to treat perimenopausal IBS, scroll down and read the following suggestions.
What Is Irritable Bowel Syndrome?
The exact causes of IBS is unknown, and yet it affects as many as 1 out of 6 people in the United States. It is a collection of chronic digestive symptoms, such as abdominal pain, gas, bloating, diarrhea, or constipation. Other conditions may cause similar symptoms, such as celiac disease, Crohn's disease, or ulcerative colitis.
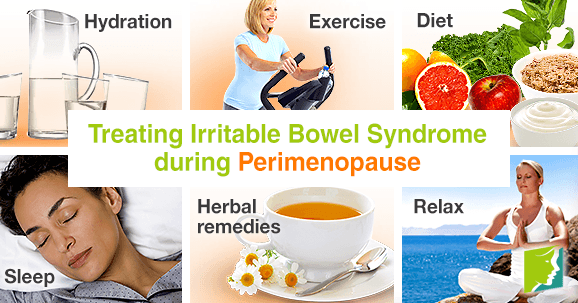
Suggestions for Treating Perimenopausal Irritable Bowel Syndrome
The best way to find relief from IBS during menopause is to cultivate healthy lifestyle habits.
Hydration. Simple but highly effective, drinking enough water can make a big difference for the gut. Water flushes the body and helps stools to pass frequently and easily. Experts suggest getting the equivalent of eight glasses of eight ounces of water each day.
Exercise. A regular regimen of moderate physical activity during menopause is not only beneficial by managing the middle-age spread, boosting mood, and tempering other menopausal symptoms, but it's also incredibly helpful against IBS. In fact, lack of activity can be the culprit behind some digestive symptoms. Cardio can help to speed up a sluggish digestive system, and strength training can improve abdominal muscle function.
Diet. Unsurprisingly, what goes into the body has a huge effect on how it performs. For sensitive digestion, consider the following:
Avoid. Too much oily or fatty food, excess sugar or alcohol, caffeine, and carbonated drinks.
Seek out. Products that contain helpful probiotics, like yogurt, as well as plenty of fibrous foods, such as fruits and vegetables, whole grains, and beans.
Sleep. Many people underestimate the power of a good night's sleep. Getting enough deep rest each night goes a long way in allowing the body to function at its best, as well as soothe the stress that is so often a major aggravator of IBS symptoms.
Herbal remedies. There are numerous herbs that have been used for centuries in calming flare-ups of indigestion, and are just as effective today. Examples include chamomile, anise, fennel, ginger, and peppermint.
Relax. The brain is linked to the intestines, which is why stress can cause abdominal pain or loss of appetite. Therefore, practices such as yoga and meditation can help both the brain and the body to relax.
Slow down. Researchers have found that taking more time to chew food is linked with better digestion, as well as other benefits like greater satisfaction, eating fewer calories, and improved nutrient absorption. It's also wise to avoid eating on the go.
Read about other ways to deal with menopausal digestive problems.
Sources
- Chevallier, A. (2000). Encyclopedia of Herbal Medicine. Dorling Kindersley.
- Longstreth, G.F. (2013). Irritable bowel syndrome. Retrieved May 29, 2015, from http://umm.edu/health/medical/ency/articles/irritable-bowel-syndrome